Your health and wellness matters. We're here to support you.
Heart of Gold is designed to support, not replace, the patient-physician relationship. Patients should always check with their doctors before making any changes in their medication or treatment.
Join Our Community
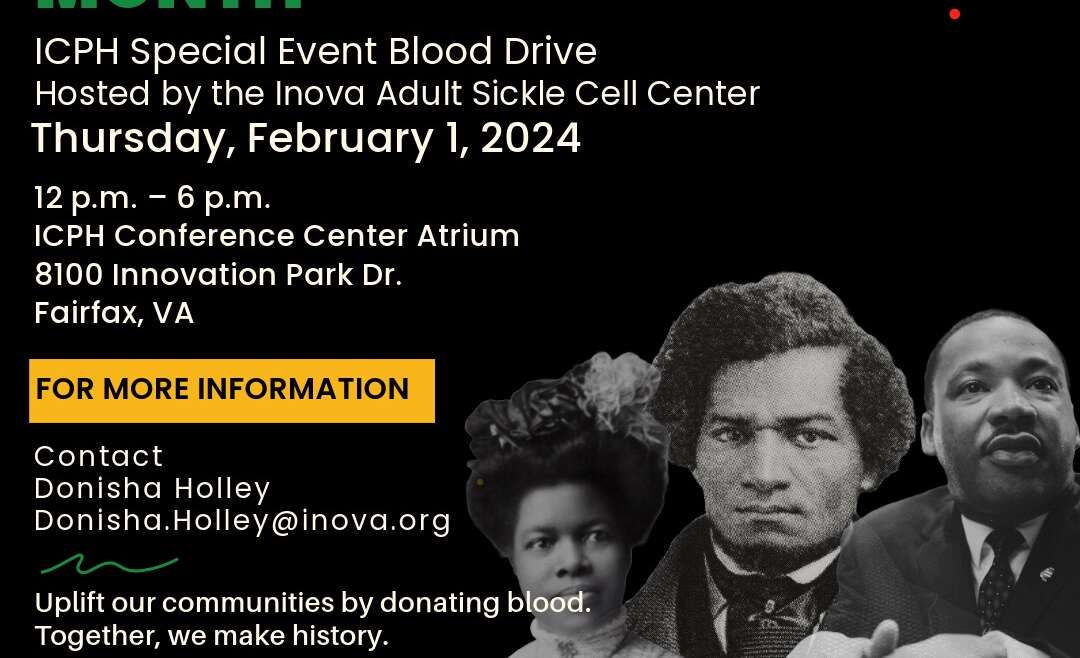
Black History Month Blood Drive. Pay homage to the past, shape the future. This Black History Month, join us in giving the gift of life through blood donation. By honoring our ancestors’ resilience, we can build a healthier, brighter…
Red Cross Blood Drive. Every donation is critical and you can make a lifesaving difference. Patients with trauma, undergoing surgery, or with conditions that require blood transfusions, such as sickle cell disease, need blood and blood products. You…
Red Cross Blood Drive. Every donation is critical and you can make a lifesaving difference. Patients with trauma, undergoing surgery, or with conditions that require blood transfusions, such as sickle cell disease, need blood and blood products. You…
Watch Our Latest Videos
The Heart of Gold Sickle Cell Foundation is a non-profit organization based in Northern Virginia. We advocate for people and their families affected by sickle cell disease. Our founder and CEO, Clarissa Pearson was born with sickle cell disease and passed away in 2021 because her body became too weak from the wear and tear of this terrible illness.
Upcoming Events
Clarissa Pearson
Clarissa Pearson passed away on March 10, 2021 a few days before her 42nd birthday. Clarissa was born with sickle cell disease, and the injuries she sustain in her life long fight eventually became too much for her frail body to endure. Never was there a true spirit of a sickle cell warrior than Clarissa Pearson. She was also a mom, daughter, cousin, friend, Non-profit CEO, AKA and much more! Her life was one of trials and suffering and hospital stays and multiple blood transfusions.
Advocacy
Whether you’re a patient, a caregiver, a friend, a family member or a provider, sickle cell advocacy is important as we work toward a universal cure. Please visit the links below to find resources to help you advocate for key legislative issues that are important to individuals living with SCD and their families.
BECOME A VOLUNTEER
If your son or daughter is under the age of 18 and would like to volunteer with the Heart of Gold Sickle Cell Foundation of NOVA, we kindly request that you fill out a parental permission form. This form ensures that we have your consent for your child's participation in our volunteer activities. You can find the form by clicking the Parental Consent Form button below. Once completed, please mail the signed form to our PO Box:
The Heart of Gold Sickle Cell Foundation of Northern Virginia P.O. Box 23681 Alexandria, VA 22304
Should you have any questions or require further assistance, please don't hesitate to contact us at 703-370-3234. We appreciate your support and look forward to welcoming your child as a valued member of our volunteer team.